The Silent Struggle: Understanding and Treating Urinary Bladder Stones
Urinary Bladder Stones: Causes, Treatments (Allopathy & Ayurveda), and Managing BPH |
| Meta Description | Comprehensive guide on urinary bladder stones: explore their formation, the role of an enlarged prostate (BPH), six major risk factors, surgical removal in men and women, and treatments across Allopathy, Homeopathy, and ancient Ayurveda. |
| Keywords | Urinary bladder stones, bladder stone causes, enlarged prostate (BPH), Tamsulosin, Flowdart Plus, cystolitholapaxy, Ayurvedic treatment for stones, urinary incontinence, bladder outlet obstruction. |
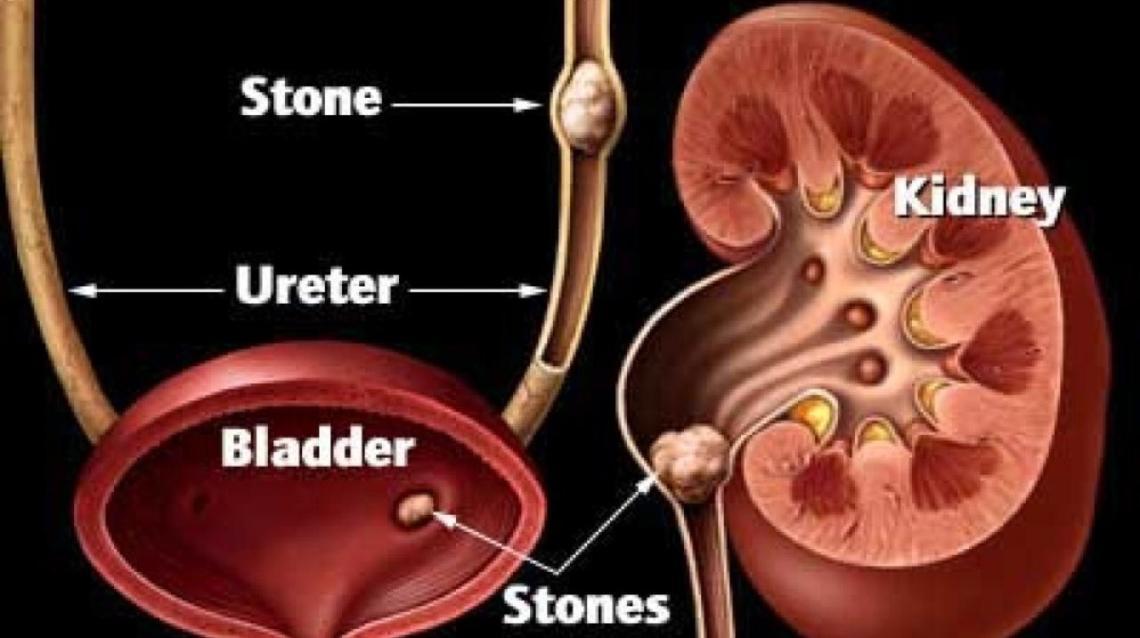
alt text urinary bladder stone shown in bladder
What Exactly Is a Urinary Bladder Stone?
ICMR Guidlines on uric acids and more external link
A urinary bladder stone, medically known as a Vesical Calculus, is a hardened mass of minerals that forms inside the urinary bladder. Unlike kidney stones, which form in the kidney and may travel down, a bladder stone usually forms in situ (in its location) when the bladder cannot completely empty, leaving behind concentrated residual urine.
These stones can range from tiny crystals that pass unnoticed to large masses the size of golf balls, leading to symptoms like lower abdominal pain, painful urination, frequent urges to urinate, and blood in the urine (hematuria).
The Roots of the Problem: Stagnation and Migration
The formation of a bladder stone is primarily linked to conditions that cause urinary stasis (urine stagnation).
1. The Prostate Connection (Men)
The most common culprit in adult men is an inflamed or enlarged prostate gland, a condition called Benign Prostatic Hyperplasia (BPH). The enlarged prostate presses on the urethra (the tube carrying urine out of the body), creating a Bladder Outlet Obstruction (BOO). This obstruction prevents the bladder from emptying fully, leaving “residual urine.” Minerals like calcium, magnesium, and uric acid precipitate and crystallize in this stagnant pool, forming a stone.
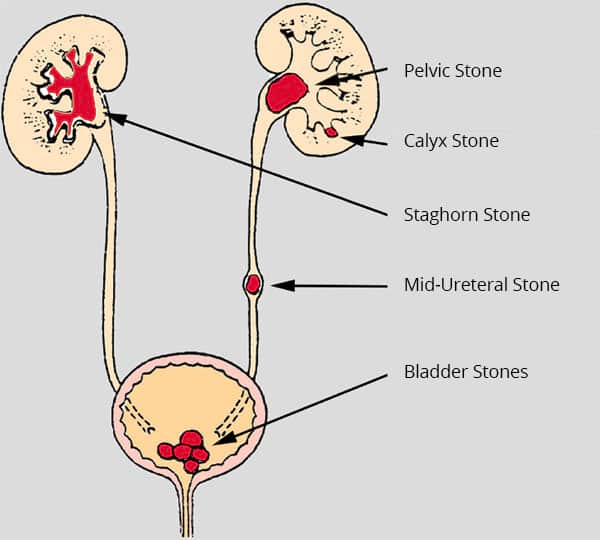
2. Kidney Stone Migration

Stone inside bladder
A stone that forms in the kidney can sometimes pass down the ureter into the bladder. While small stones are usually flushed out, a larger kidney stone can get stuck in the bladder and act as a nidus (a nucleus or seed) for other minerals to deposit upon, quickly growing into a larger bladder stone.
6 Major Factors That Cause Stone Formation
Beyond BPH and kidney stone migration, several other conditions can cause urinary stasis or inflammation, leading to stone formation:
* Neurogenic Bladder: Nerve damage (from stroke, spinal cord injury, or Parkinson’s disease) prevents the bladder muscle from contracting correctly, resulting in incomplete emptying.
* Foreign Bodies: Medical devices like long-term catheters or surgical sutures can act as surfaces where crystals rapidly deposit and grow.
* Chronic Urinary Tract Infections (UTIs): Persistent infections, particularly those caused by urea-splitting bacteria, can raise the urine’s pH, leading to the formation of Struvite stones.
* Urethral Strictures: Narrowing of the urethra due to injury or infection causes a blockage, leading to urinary retention.
* Bladder Diverticula: Small pouches or pockets that form in the bladder wall trap urine, creating stagnant pockets ideal for stone formation.
* Cystocele (Dropped Bladder) in Women: When the bladder prolapses (drops) into the vagina, it can kink the urethra and obstruct the flow, leaving residual urine.
Why Women Have Bladder Stones (No Prostate Damage)MOHFW guidlines on health read more
As noted above, while BPH is the primary cause in men, women are equally susceptible through other mechanisms. Since the female urethra is short and wide, stones that do form are often flushed out.
However, factors like Cystocele (bladder prolapse after childbirth), neurogenic bladder (nerve damage), bladder diverticula, and most commonly, recurrent or chronic UTIs and inflammation are the major driving forces for bladder stone formation in women.
Surgical Removal: How Operations Differ
The primary modern allopathic procedure for stone removal is called Cystolitholapaxy (or percutaneous cystolithotripsy for very large stones).
* For Men: The surgeon inserts a rigid or flexible instrument (cystoscope) through the penis/urethra into the bladder. The instrument is used to visualize the stone, break it up with a laser or ultrasonic device, and then wash out the fragments.
* For Women: The procedure is similar (Cystolitholapaxy) and is generally easier to perform because the female urethra is significantly shorter and straighter, providing more direct access to the bladder. Open surgery is rare today, reserved for extremely large or complicated cases.
A Multi-Faceted Approach to Treatment
Allopathic (Modern) Medicine
* Medical Dissolution: Used primarily for uric acid stones, involving oral medication to alkalize the urine.
* Surgical Intervention: Cystolitholapaxy (as described above) is the mainstay of treatment.
* Management of Underlying Cause: Medications like alpha-blockers or 5-alpha-reductase inhibitors are prescribed to treat BPH and prevent recurrence.
Homeopathic Medicine
Homeopathy focuses on individualized treatment aimed at dissolving the stone and treating the underlying constitutional tendencies. Remedies often suggested include Sarsaparilla, Berberis Vulgaris, and Lycopodium to help relieve renal colic, improve urination, and assist in passing small fragments.
Ancient Ayurvedic Medicine
In Ayurveda, urinary stones are termed Ashmari (Ashma = stone, Ari = enemy).
Sushruta and Charaka’s Teachings
The ancient texts describe two main approaches:
* Acharya Charaka (Physician): Focused on Shamana Chikitsa (conservative, palliative treatment) using herbal medicines with diuretic (mutrala), stone-splitting (ashmaribhedana), and alkali (kshara) properties.
* Acharya Sushruta (Surgeon): Recognized as the Father of Indian Surgery, he described both conservative medicine and Shastra Karma (surgery). He pioneered perineal cystolithotomy—surgical removal of the stone through an incision in the perineum (the area between the anus and scrotum/vagina)—if conservative treatment failed.
Commonly used herbs and compounds for Ashmari include Varuna (Crataeva nurvala), Pashanbheda (Bergenia ligulata), Gokshura (Tribulus terrestris), and Yavakshara (medicated alkali preparation).
The Brain-Bladder Connection and Incontinence
When an enlarged prostate (BPH) obstructs the urethra, the bladder muscle (detrusor) works harder to push the urine out, leading to muscle thickening (hypertrophy). Over time, this chronic strain can damage the nerves and muscle, causing the bladder to become hypersensitive or weak.
This constant irritation sends misfiring signals to the brain, leading to an uncontrollable, sudden urge to urinate—known as Urge Incontinence. When the muscle fails completely, the bladder overstretches, and urine leaks out when the bladder is overfull, known as Overflow Incontinence. The brain has essentially “lost control” because the chronic physical obstruction has disrupted the normal nerve reflex pathway.
Unpacking Flowdart Plus
Flowdart Plus is a common medication prescribed in the early to mid-stages of BPH.
* Active Salt Ingredients:
* Tamsulosin (0.4mg): An alpha-1-blocker that works instantly by relaxing the smooth muscles in the prostate and the neck of the bladder. This reduces resistance and allows urine to flow more easily.
* Dutasteride (0.5mg): A 5-alpha-reductase inhibitor that works slowly by blocking the hormone (DHT) responsible for prostate growth, thus shrinking the gland over time.
It is prescribed at the first stage to provide both rapid relief (Tamsulosin) and long-term size reduction (Dutasteride). The assertion that “incontinence is maintained at a faster rate” is generally inaccurate. The medication is intended to relieve symptoms like frequency and urgency (a type of incontinence). If incontinence persists, it’s usually because the bladder muscle or nerve damage is already advanced, requiring additional treatment.
Dietary Adjustments for Prevention
While hydration is key to diluting minerals, dietary changes beyond restricting salt and refined sugar are necessary:
* Limit Excessive Animal Protein: High intake, especially of red meat and organ meats, increases uric acid levels, promoting the formation of uric acid stones.
* Moderate Oxalate-Rich Foods: If you have calcium oxalate stones, reduce high-oxalate items like spinach, rhubarb, beets, almonds, and chocolate.
* Avoid Excess Caffeine and Alcohol: These can act as diuretics, leading to dehydration and more concentrated urine.
* Ensure Sufficient Citrate: Foods rich in natural citrate, like lemons and oranges, can help inhibit stone formation.
Disclaimer: This blog post is for informational and educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider or a licensed practitioner of Ayurvedic or Homeopathic medicine with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen.
Internal link https://dailydrdose.com